With many people implementing new exercise programs as a New Year’s resolution, it seems best to focus this discussion on the role of the pelvic floor and how it relates to choosing the type of exercise that’s best for you.
As a physical therapist and a certified pelvic rehabilitation practitioner (PRPC), I work with a large variety of medical diagnoses, including issues not always easy to discuss, such as urinary and fecal incontinence, painful sexual intercourse, pregnancy/postpartum conditions, pelvic organ prolapse, post-hysterectomy issues, adult and pediatric urinary and bowel disorders, and female and male chronic pelvic and abdominal pain syndromes.
The most important thing to know is there is no “cookie cutter” approach to treating pelvic floor dysfunction, because no two pelvic floors are exactly alike.
The Pelvic Floor and Its Functions
The pelvic floor consists of several layers of muscles and fascia that span the bottom of the pelvic cavity, much like a hammock or sling, connecting the pubic bone in front to the coccyx bone (also known as your tailbone) in back, as well as other layers, which are more circular and sphincteric in nature.
These muscles contribute to five main functions of the pelvic floor:
- Support of the pelvic organs, including the bladder, uterus and colon.
- Assist in stopping and starting the flow of urine and the passage of gas or stool.
- Aid in circulation, and in muscle contractility for sexual appreciation and orgasm response.
- Aid in core stability of the pelvic girdle.
- Aid as a “sump pump” for the lymphatic and circulatory system.
The average individual is only vaguely aware they have a pelvic floor, typically through being briefly instructed to “do your Kegels” to prevent urinary leakage and improve sexual function.
The term “Kegels” describes the squeezing and lifting motion of the pelvic floor. The exercises were named after physician Arnold Kegel, who patented specialized biofeedback equipment in 1948 to study the relationship between continence and pelvic floor weakness in women. As grateful as the practitioners of my profession are to the groundbreaking work of Kegel, you will often hear us emphatically state, “Pelvic floor physical therapy is so much more than Kegels.”
Understanding Your Pelvic Floor Type
According to the International Continence Society Standardization of Terminology of Pelvic Floor Muscle Dysfunction, there are four distinct presentations found when evaluating a pelvic floor:
- A normal functioning pelvic floor is one that is able to contract and relax on command and to respond appropriately to increases in intra-abdominal pressure, such as coughing, laughing, sneezing, lifting, etc.
- An underactive pelvic floor is one which is unable to contract appropriately or to generate enough force to lift against gravity, and lacks adequate coordination and timing to perform properly.
- An overactive pelvic floor is unable to relax on command and may involuntarily contract during normal bodily functions such as urinating and defecating, when ideally the pelvic floor should be relaxed.
- A nonfunctioning pelvic floor is one which is unable to generate any voluntary muscle contraction or relaxation.
Exercise and Therapy for the Pelvic Floor
It is very important to know what type of pelvic floor you have before embarking on any new exercise program, because what is beneficial to one pelvic floor may be harmful to another. This is where the role of a pelvic floor physical therapist is key.
A physical therapist that specializes in treating pelvic floor dysfunction is uniquely trained in evaluating and palpating the joints, ligaments and internal soft tissues (muscles/fascia/nerves) that comprise the pelvic floor and pelvic girdle complex, and in identifying abnormalities and asymmetries in the soft tissue.
For example, person “A” may have an overactive pelvic floor with short, tense muscles, as opposed to person “B” who may have an underactive pelvic floor which is over-lengthened or stretched. Both scenarios are considered weak and dysfunctional, but the recommended treatment would be different.
To complicate matters, sometimes an individual will have an asymmetrical pelvic floor, with one side shortened, tight and overactive, and the other side nonfunctioning or overstretched/lengthened. This is why an internal evaluation and proper assessment of the pelvic floor is ideal, as the exercise prescription for different pelvic floor conditions will vary significantly.
Just as no two pelvic floors are the same, no two people learn exactly the same way. Throughout my 15 years as a pelvic floor physical therapist, I have incorporated catchy phrases and utilized imagery and analogies to teach proper function of the pelvic floor.
Relaxing your pelvic floor is just as important as contracting it. Unfortunately, this principle is often overlooked, and many are instructed to do repetitive “Kegels” with no clear explanation of how to do them correctly and how many to do. Contrary to popular belief, Kegels are not appropriate for everyone. Unfortunately, few people are given a muscle exam to discern whether Kegels are appropriate for their particular pelvic floor condition – and repetitive Kegels should never be performed in the presence of pain, a spasm, or during a urinary tract infection.
If someone has a tight pelvic floor, pain or trigger points, then doing Kegels can be harmful because they make muscles that are already too tight even tighter, and can exacerbate trigger points. A pelvic floor therapist is trained to palpate for areas of tenderness, scar tissue and nerve sensitivity which may need to be addressed before pelvic floor strengthening is even recommended.
When it comes to your pelvic floor, it is important to remember that “less is more.” It’s not about how strong your muscles are – what is more important is having the correct motor control to be able to use the right muscles at the right time and in the right order.
Individuals with pelvic pain and hypertonic pelvic floor muscles need to start with relaxation to gain length of the pelvic floor muscles before implementing strengthening of the pelvic floor. Pelvic floor voluntary lengthening is necessary in order to be able to relax to fully empty our bladder and bowels, and to allow for entry during sexual intercourse.
Most importantly, remember that pelvic floor muscles are very much connected with our emotions. Chronic anxiety and stressful situations contribute to faulty holding patterns and short, tense muscles. Because of this, generalized programs incorporating strengthening and repetitive core training without lengthening can be detrimental and often exacerbate pelvic pain conditions.
Your pelvic floor is the very foundation of your “core.” Pelvic floor exercises should be applicable to daily life – a strong core protects your organs during exertion (pushing, pulling, lifting, bending, coughing and sneezing) and aids in prevention of pelvic organ prolapse and other supportive dysfunctions.
Exercise programs that include repetitive jumping and high-impact maneuvers are cautioned against for individuals with pelvic organ prolapse conditions, underactive pelvic floor muscles, or ligamentous laxity.
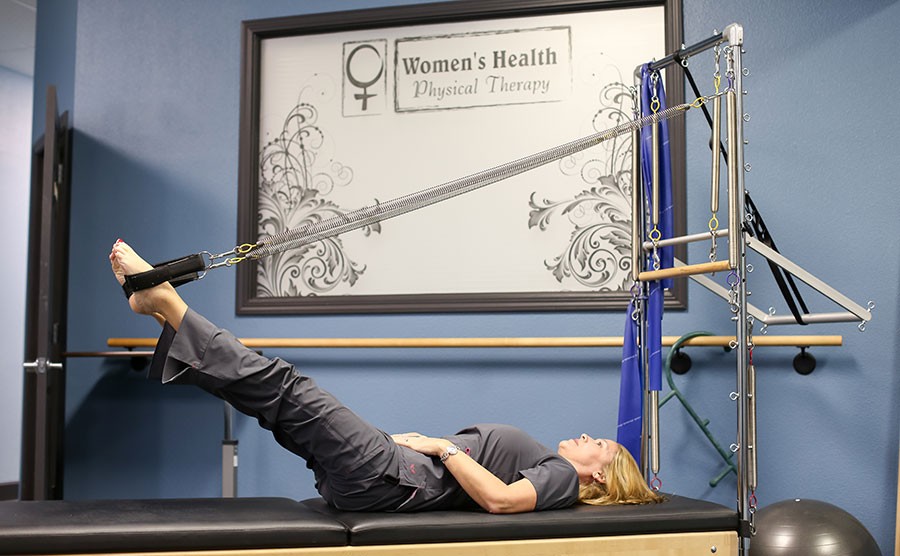
An evaluation by a specialized pelvic floor therapist will help guide you in making the correct choices when deciding which type of generalized exercise program is best for you and your pelvic floor. There are many specialized forms of exercise, including yoga, Pilates, CrossFit, Curves, and Boot Camp, many of which address core strengthening, and some which focus on lengthening the pelvic floor as well. Choose exercise programs and professionals who are mindful of the role of the pelvic floor and are willing to work with your individual limitations.
If you are at all concerned about potential pelvic floor problems, I strongly recommend you consider asking your primary care physician, obstetrician or gynecologist for a referral to a pelvic floor physical therapist before embarking on a new exercise program. Having a good understanding of your unique foundation will help guide you in making the wise choice for your long-term health. When it comes to the pelvic floor, prevention is paramount and can best be achieved by developing good pelvic floor habits.
For further information on the topic, or to find a practitioner in your area, consider the following references and resources:
- The Section on Women’s Health of the American Physical Therapy Association
- The Herman & Wallace Pelvic Rehabilitation Institute
- The Pelvic Health and Rehabilitation Center
- The International Continence Society
- The International Pelvic Pain Society
Posted in: Health & Nutrition
Comment Policy: All viewpoints are welcome, but comments should remain relevant. Personal attacks, profanity, and aggressive behavior are not allowed. No spam, advertising, or promoting of products/services. Please, only use your real name and limit the amount of links submitted in your comment.
You Might Also Like...

Brande Moffatt & Women’s Health Physical Therapy – A Passion For Helping Women
The founder and owner of Women’s Health Physical Therapy in Redding, CA, and a Certified Pelvic Rehabilitation Practitioner, Brande Moffatt, PT, MPT, PRPC, is uniquely qualified to help women recover from […]

Shasta Community Maternity Center
A Warm Hug of Services The healthcare team at Shasta Community Maternity Center wants every woman to feel as though she’s wrapped in a warm hug of quality services each […]

Back to School and Back to Packing Lunches?
Consider these reusable, chemical-free sandwich and storage bags for the kids — and anyone who brings their lunch to school or work! ReZip is food safe, leakproof, lightweight and can […]

Home Visit Programs Link New Mothers With Experienced Nurses
When she found out she was pregnant, Sarah says, “I didn’t really know what to do. (My baby’s) father passed away before he was born, and I was recovering from […]